What the heck is ACT? If you find yourself thinking, “another type of behavioral therapy? Another acronym?!” I would get it. It’s true, as a therapist, I geek out on this stuff. But I wouldn’t write a blog post about it if I didn’t think it was really worth your time.
So what is it? ACT is all about accepting what is out of your personal control and committing to action that enriches your life. What do you want to stand for in your life? What truly matters to you? Once you clarify your core values you can use them as guides to motivate and inspire behavioral change.
- Accept your thoughts and feelings, and be present
- Choose a valued direction
- Take action
How is this different from other types of therapy? We are often being sent messages about the need to control our emotional states. Think about the self-help section in a bookstore: You see titles like “How to Feel Less Stress” or “5 Ways To Find Happiness.” At some point, all of us probably received feedback about getting over an unpleasant emotional state. It’s what I like to call the wipe off your knees and keep going mentality. When we buy into this, we tell ourselves we’re not doing a good enough job– if we feel too much stress, anxiety, fear, shame, guilt, and not enough happiness or joy. When we internalize these messages we try to control our thoughts and feelings. In ACT, we believe that thoughts and feelings themselves are not pathological. We don’t need to chase them down and change them. Rather, the focus is on relating to them in a different way by accepting their presence, fully and without defense, and choosing what you will or won’t do based on your personal values. It sounds nice, but how do we actually put that into practice? In ACT, there are six core processes that can help guide you: defusion, self-as-context, presence, acceptance, values, and committed action. Each of these processes comes with a number of different skills. For this blog post, I will explain each step and scatter into some exercises.
Defusion:
We get caught up in our thoughts; we take them as capital “T” truth and often see the world through the lens of a painful thought we have about ourselves, others, or the world. Defusion is about stepping back and detaching from inner thoughts or images. Instead of getting caught up in our thoughts, we let them come and go. We see thoughts for what they are– nothing more or less than words or pictures. We hold them lightly instead of clutching to them tightly.
Exercise: Take a painful thought such as, “I’m unlovable” and get a bit of space from it by inserting one of the clauses below:
- “I’m having the thought that [“I’m unlovable]”
- “When I experience the emotion [shame], my mind tends to tell me [“I’m unlovable”]
- “The story I tell myself is [“I’m unlovable”]
The Observing Self (also known as Self-as-context):
There are two elements of the mind: The thinking self and the observing self. The thinking self is the part of us that is always thinking– generating judgments, fantasies, beliefs, and so on. The observing self is less talked about in our culture. This is the part of us that is aware of whatever we’re thinking, feeling, sensing, or doing in any moment. Throughout life your body, thoughts, roles, and feelings all change but the “you” that’s able to notice or observe all those things never changes.
Contact the present moment
Our judgmental, problem-solving minds constantly pull our attention away from the present. Why? We want to avoid suffering and we yearn for orientation– to know where we are in our life journey. But instead of orienting ourselves, we end up ruminating about what’s happened in the past or worry about what will happen in the future. Both of these “thinking self” processes are associated with depression and anxiety. Contacting the present moment is about mindfulness, defined as “paying attention in a particular way, on purpose, in the present moment, and non-judgmentally” (Jon Kabat-Zinn).
Exercise: Try this simple 6-minute meditation
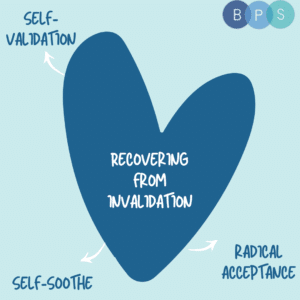
Acceptance:
When we try to avoid uncomfortable thoughts and feelings, we demonize natural human experiences. Our efforts, energy, and attention are spent trying to control unwanted inner experiences and we feel even worse when they show up. Avoidance is not workable as a long-term solution. As we say in ACT:
If you don’t want it, you’ve already got it.
If you aren’t willing to be anxious, you will feel even more anxious.
If you aren’t willing to feel pain, you will feel even more pain.
If you keep doing what you’re doing, you’ll keep getting what you’re getting.
The goal of acceptance is a willingness to make room for uncomfortable feelings, sensations, urges, and emotions. Instead of struggling against them, we open up to them and let them be. This does not mean you have to like it or want it (anxiety IS uncomfortable), but it’s about allowing yourself to have it. In fact, the wisdom of pain is that it tells us what matters most. For example, I might feel pain if a friend is upset with me or I might feel anxiety after a social interaction. What those uncomfortable emotions tell me is that I don’t want to hurt my friends or that I care about how I’m perceived in social situations because connection matters to me. Values and vulnerabilities are two sides of the same coin; the more we pursue our values the more vulnerable we will feel.
Exercise: Say “Yes”
Consider a painful thought or memory that you often struggle with or avoid altogether. Put a 1-minute timer on. Close your eyes and adopt a “no” stance towards that thought or memory as in: “No, that’s not good. That needs to change; that is unacceptable.” Allow yourself to struggle against it as you normally do. When the timer goes off, note any observations of what that experience was like: What emotion did you feel? How did you hold your body (tense, relaxed)? What happened in your mind (did your thoughts speed up? Slow down?) Next, put the timer on again for 1 minute. This time, take that same thought or memory but instead adopt a “yes” stance towards it as in: “yes, I am willing to allow that to be there, just as it is. I do not need to change it.” Afterward, observe or describe how these experiences were different.
Values
In ACT, we define values as qualities of being. For example: Being a loving, caring, attentive, curious, and supportive partner.
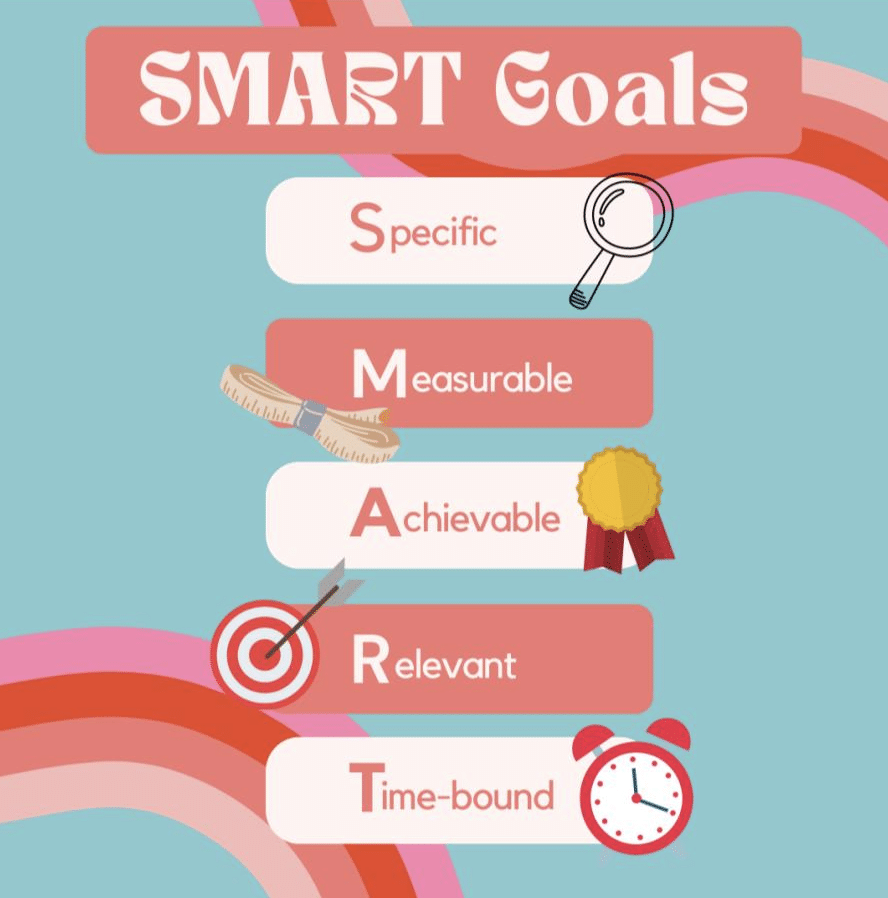
Values are not goals. Goals can be met, checked off a list, or completed. Values are what we live by and we continuously commit and recommit to them. I can meet my goal of getting married but I’m never done being a loving partner. Love is ongoing. It matters before and after you get a partner.
The more in touch we are with what truly matters, the easier it is to take a step in the right direction.
Exercise: Attend your own funeral
Close your eyes and take a few deep breaths to calm your mind. Picture witnessing your own funeral. Think about where it would be and visualize a clear picture of your funeral service in your mind. Imagine that a loved one is saying a few words about what you stood for in your life; about what you cared about. Write out what you would want to hear in your eulogy about how you lived your life. Notice if certain thoughts or judgments come up. Defuse from them. This is not a prediction of your life but rather a reflection on the meaning you would most like to create; the purpose you would most like to reveal about the time you spent on this planet.
Committed Action
Take effective action towards upholding your values. Value-guided action gives rise to a wide range of thoughts and feelings– both pleasurable and painful. Committed action means doing what it takes even if it brings on pain and discomfort. Maybe I’m terrified to open up fully in a relationship; to be vulnerable. I could choose to avoid that feeling by saying no to dates, being hypercritical of someone I meet, or closing myself off from someone emotionally, but that won’t help me get to where I want to go (having a close, connected, intimate relationship). Instead, what do I do? Committed action often encompasses all other act processes: Download the dating app (action), defuse from self-critical thoughts, accept the anxiety you feel, observe fear and shift towards curiosity and openness (values), show up fully present, with the intention of getting to know someone.
Putting it all together:
One quick way to put it all together yourself. If you find that you’re in a situation and struggling with your inner world, ask yourself these questions:
- What is the story I am telling myself in this moment? (e.g. the story of no one likes me)
- How do I react when I buy into that story? (e.g. get quiet, retreat, internally criticize everything I do)
- Who or what is important to me right now? (e.g. getting to know someone, connecting, being present)
- What are some actionable steps towards that? (e.g. find someone approachable, sit and ask them questions, listen intently)
Now you try!